Aortic coarctation is a narrowing of a portion of the aorta, the major artery that leads out of the heart to the body. This narrowing usually occurs at the point of curvature of the aorta, just beyond where the branches that supply the arms and head leave. From the curved portion, the vessel extends downward into the abdomen and supplies blood to the lower half of the body.
No one knows exactly what causes aortic coarctation. But changes in another blood vessel – the ductus arteriosus – and its related tissues may be responsible for development of the condition. Almost all coarctations occur at the site of insertion of the ductus arteriosus, which functions in the fetus to divert blood from the heart back to the placenta. In effect, this blood vessel serves as a bridge between the artery that takes blood to the lungs (the pulmonary artery), and the aorta, which takes blood to the body. The ductus arterious normally closes after the baby is born.
Coarctation often becomes symptomatic with the disappearance of the ductus arteriosus. In some babies, coarctation can lead to development of shock, because of both inadequate blood flow to the abdominal organs – and everything else below the level of the narrowing – and extra pressure that’s placed on the heart from the blockage.
Coarctation is rarely detected in the fetus, but can become evident in infancy or at an older age. Most physicians who see older children or adults with aortic coarctation believe they had it very early on, but the degree of narrowing was not significant enough to cause problems, and it therefore missed detection. In patients with coarctation of the aorta, the body develops alternative pathways to get the blood beyond that area of narrowing. These may enlarge significantly over time. The medical term that’s used for this is “collaterals.” Older patients who have coarctation often have evidence of large collaterals.
The consequence of coarctation is higher blood pressure upstream from the narrowing and decreased blood pressure downstream from the narrowing. In response to this, the kidneys secrete hormones to try to regulate blood flow. If coarctation is treated in later childhood or adolescence, it is less likely that high blood pressure can be resolved, even after the coarctation is treated, because of permanent changes that take place in the vascular system. Adults who have had longstanding coarctation can also develop aneurysms in their brains called “berry” aneurysms. That’s why patients with coarctation require lifelong surveillance by their cardiologists.
Coarctation can also be associated with other heart problems or defects. In some patients, coarctation can occur in conjunction with other left-sided heart lesions, in particular defects of the aortic or mitral valve. For example, the association of bicuspid aortic valve and coarctation is common. The presence of coarctation can impact the function of these valves and potentially lead to more problems. That is why it’s critical to treat coarctation once it’s identified.
The nature of the coarctation can vary. In most cases, the narrowing has a very short length or is “discrete.” In other cases the narrowing can extend for a longer length of the aorta. Specifically, there can be underdevelopment of segments of the blood vessels upstream from the area of narrowing. This is important because it helps determine what treatment may be most effective.
Treatment
The standard approach for coarctation – particularly when identified in neonates and younger patients – is surgical. On occasion, nonsurgical, catheter-based interventions are used.
There are no medications that can help resolve coarctation. Sometimes medicines are used to reduce the effects of coarctation, specifically to treat high blood pressure or related heart problems. Yet even in those circumstances, medical therapy is typically done in concert with surgical therapy. At the same time, less-invasive, catheter-based interventions have been developed to treat some cases of coarctation.
Typically, in the newborn period, if there is significant narrowing of the coarctation, immediate operation is recommended. If there are extenuating circumstances that increase the risk of surgery, and the child appears to have at most a mild to moderate degree of coarctation, we would consider delaying the operation until the risk is reduced. Alternatively, if there are other heart-related conditions that required surgical therapy, these might influence the decision to proceed with surgery.
The standard approach for discrete aortic narrowing is via an incision between the ribs on the left side of the chest. The aorta sits very far back in the chest cavity next to the spine. Surgeons spread the ribs apart, push the lung out of the way, open up the lining inside the chest that overlies the aorta and, after exposing the aorta, isolate the segment of narrowing between clamps. They then cut out the segment and sew the two ends of the aorta together, usually overlapping the segments to address any milder narrowing of the adjacent segments of the aorta.
The operation usually takes 2-3 hours. The portion of the operation in which the segment is cut out and the two ends are brought together is typically 15-20 minutes. A small amount of blood thinner called heparin is given to prevent clot formation downstream from where the aorta is clamped.
For the 15-20 minutes during which the segment of narrowing is isolated, there may be decreased perfusion to the lower part of the body and increased perfusion, or higher pressure, to the upper part of the body. The lower body is typically adequately supported with blood for this short period via the collateral blood vessels described previously. Our anesthesiologists are trained in managing children’s cases and know how to ensure the patient is well protected during the operation.
There are variations of how the two portions of the aorta are connected depending on the degree of underdevelopment of the upstream portion of the aorta. If the narrowing is discrete, and the degree of underdevelopment is minimal, then the extent that the lower aorta is brought up and attached to the underside of the arch is pretty minimal. On the other hand, if there is more extensive narrowing, a larger portion of the aorta is opened up or sometimes the aorta is patched, typically with a native blood vessel that takes blood to the left arm.
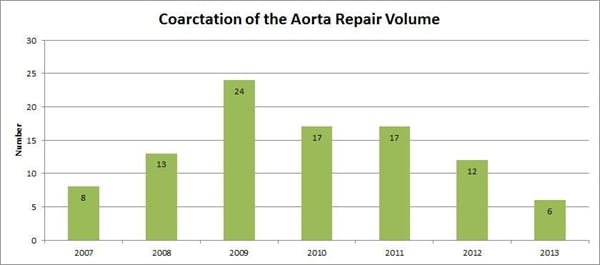
About 50% of the children who undergo coarctation repair are treated within the first few months of life. The age of repair for the other 50% spans a wide range, though most cases are identified and repaired during childhood. On rare occasion, adults whose condition has gone undetected undergo an operation. However, most adults have had some kind of previous intervention and have residual coarctation or associated problems.
On occasion, it may be necessary for surgeons to use a form of cardiopulmonary bypass support for repair of a coarctation.This is to more safely perfuse those parts of the body that would otherwise not be getting as much blood. With neonates and infants, this is almost never needed unless the coarctation is more extensive or is being done along with other open-heart repair procedures. Babies have an excellent circulatory system that accommodates the brief period of interruption in circulation to the lower part of the body required for the surgery. In general, this is around 15-20 minutes.
An exception to this in neonates and infants would be cases in which the narrowing is associated with other heart defects that require simultaneous repair, or when the degree of upstream underdevelopment is so extensive that the surgeon is not just cutting out a small portion of the aorta, but rather is performing an arch reconstruction.
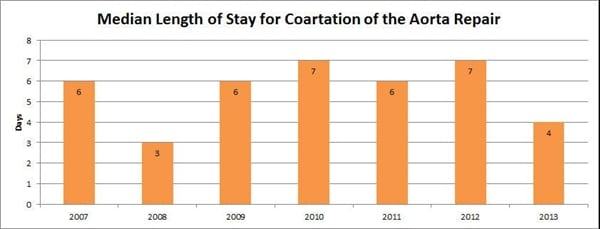
Coarctation repair is a commonly performed operation with very good results. Typically, children are in the intensive care unit for 1-2 days and spend an additional 2-4 days in the hospital.
Complications
Complications include the risk of bleeding, although it’s rare for children to require any blood transfusion. There is some risk of injury to a nerve that goes to the left vocal cord, called the recurrent laryngeal nerve. This nerve wraps around the ductus arteriosus; very rarely, with the surgeon working around that area, the nerve can become bruised. It is exceedingly rare that the nerve is permanently damaged. Most of the time, the nerve recovers, but it can take some time for recovery to take place. The injury typically causes hoarseness.
Another rare complication is chylothorax, the buildup of lymphatic fluid (chyle) – a milky white fluid – in the space around the lungs. Chylothorax happens in about 1-2% of cases; it can lead to an extended hospital stay, sometimes in the order of 3-4 weeks.
Re-coarctation
The most significant risk of coarctation repair, although not a very high one, is that of re-coarctation, or re-narrowing. This can occur in anywhere from 2-10% of children after coarctation surgery, with statistics indicating the risk of re-narrowing is greater in younger children. Historical data suggest that babies under three months of age had a 25% incidence of re-coarctation. More current experience suggests a lower incidence of around 2-5%.
Fortunately, the vast majority of re-coarctations can be treated with a catheter-based approach (balloon angioplasty). This approach is typically not used as the primary treatment for significant coarctation because of the complications that can develop from using a catheter on a native coarctation. However, once a repair has been done, balloon angioplasty is quite effective in treating re-coarctations that occur at the site of the scar tissue.
Postoperative care
The thoracotomy that is used as the standard approach to coarctation repair is, surprisingly, more painful than a sternotomy, in which a vertical inline incision is made along the sternum. A number of different steps are taken to address the pain. Epidural catheters are sometimes used. Alternatively, numbing medicine is put between the ribs to temporarily anesthetize the nerves that course through the area. Supplemental pain medicine can be given either by IV or orally. Typically by the time children go home, most are not on any pain medication.
There is no need for modification of diet unless the child has chylothorax. Most children don’t have much food intake for the first few days after the operation. But they start progressing on their diet once that time period has passed. If newborns have not learned to feed, they may require a little more time to get them in a routine.
Most patients, particularly neonates or infants, do not require additional medication after coarctation repair. Older patients, particularly those with high blood pressure before surgery, will require blood pressure medications for a time following the operation, and in some cases, these may need to be continued indefinitely.
Because of the risk of re-coarctation, it’s important for patients to have continued follow-up with their cardiologist. Most re-coarctations occur within a year after the original operation. The cardiologist checks blood pressure and may do an echocardiogram evaluation of the reconstructed aorta. They may make recommendations about activity restrictions based on any residual cardiac or aortic abnormalities that exist.
Most children with good results from surgery can be active and expect normal life expectancy with no specific physical limitations, as long as there are no other associated heart problems. Although patients require lifelong surveillance, coarctation repair can be a very effective surgery with lasting results.